Definition
What is a prostatectomy and when is it an option?
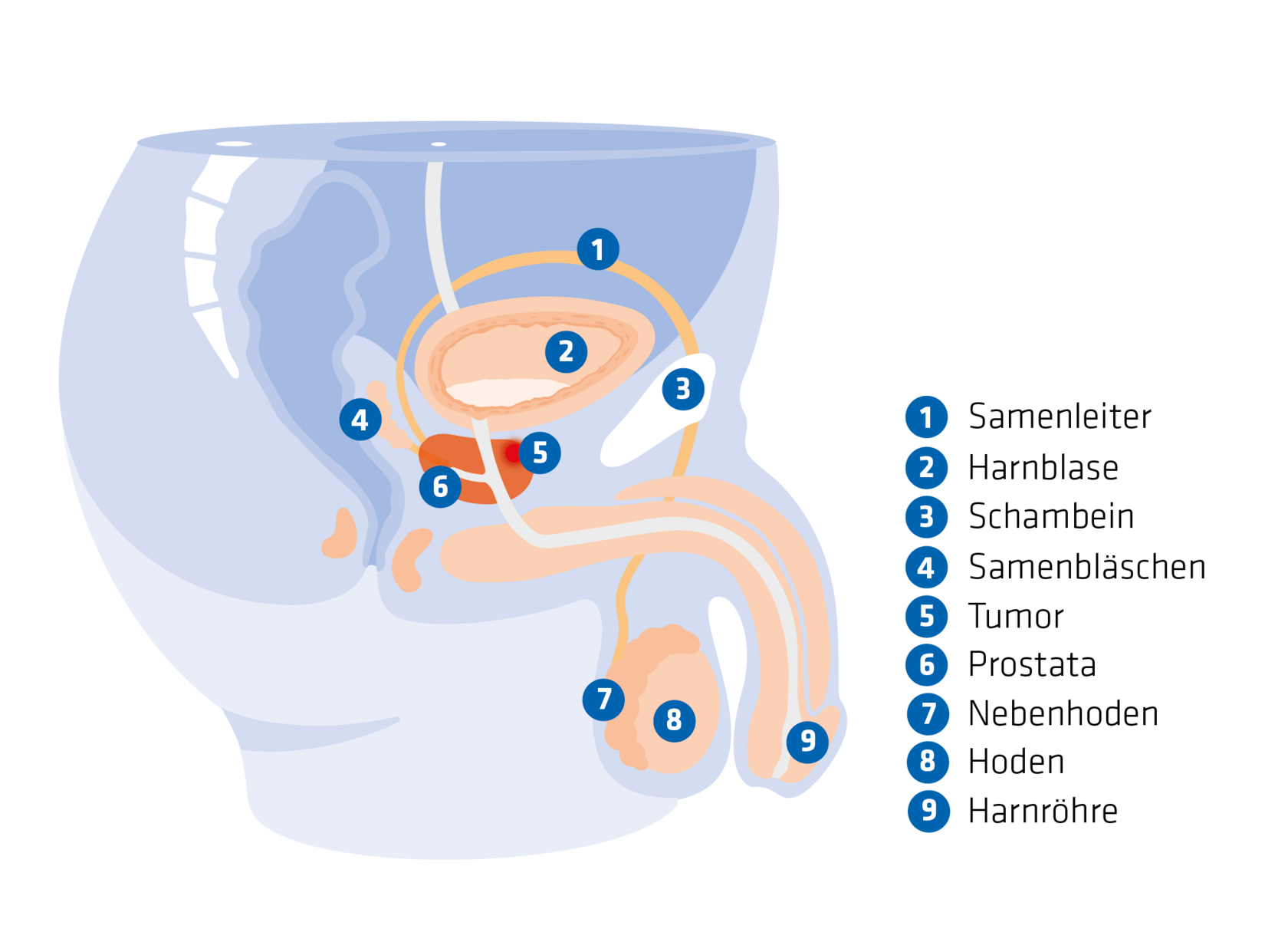
Radical prostatectomy, or RPE for short, is a surgical procedure tocompletely remove the Prostate. This type of prostate surgery is suitable for patients with prostate cancer where the cancer is confined to the prostate and has not yet spread (metastasised).
Doctors may also consider a prostatectomy for locally advanced prostate cancer that has already penetrated through the prostate capsule. In such cases, however, the risk of the disease relapsing must be carefully considered. If several lymph nodes are affected by cancer cells, the risk of relapse is high, which makes radical prostatectomy a less likely option. If there is a risk that all the tumour tissue cannot be removed, then other treatment options are used. If surgery is nevertheless performed, it is usually followed by radiotherapy.
The aim of prostate surgery is to cure prostate cancer by removing the organ and neighbouring tissue (sometimes even the affected lymph nodes). Prostate removal is considered successful if a histological examination does not show any more cancer cells at the edges of the incision. Experts refer to this as "R0 resection".
Procedure
Prostate removal can be performed in different ways depending on the access point. Open surgical methods include
- Retropubic: In this method, a longitudinal incision is made in the lower abdomen between the navel and the pubic bone. This technique is also known as "open RPE".
- Perineal: The incision is made between the anus and the penis. However, the lymph nodes cannot be removed simultaneously in this method.
Minimally invasive methods include
- Laparoscopy: In this so-called "keyhole surgery", small incisions are made in the abdominal wall, which are between 5 and 12 mm in size.
- Robot-assisted laparoscopy: A robot is used during the surgery. The device does not operate alone, but supports the surgical team, which can remove the prostate gently and quickly.
Preparation for prostate surgery
Once prostate cancer is diagnosed and the decision is made to undergo a prostatectomy, the patient can start preparing physically and mentally for the surgery. Help such as instructions for strengthening the pelvic floor muscles or psycho-oncological care can be considered here. In addition, actively dealing with the disease helps one to come to terms with the diagnosis which is often life-changing and frightening.
The patient is admitted to hospital the day before the surgery.
There is a consultation with the anaesthetist during which questions about allergies and intolerances to anaesthetics are clarified. The patient is also informed about the potential risks of the anaesthetic.
This is followed by a consultation with the surgeon, who explains the planned procedure and the associated risks and consequences to the patient. After the consultations, the patient has to give a written consent for the prostate surgery and the anaesthetic.
![[Translate to English:] Arzt veranschaulicht Ablauf der Prostatektomie mithilfe eines anatomischen Modells.](/fileadmin/_processed_/a/7/csm_AdobeStock_752001824_864e6ff07b.jpg)
Surgical procedure
The surgery itself takes about 2 hours - if lymph nodes are also removed, then about 3 hours. Depending on the procedure chosen, the patient either lies on the back or in the so-called lithotomy position (with lower legs resting on supports and legs spread apart).
This is how the prostate removal procedure works:
- After making the skin incision, lymph nodes near the prostrate are first removed (lymphadenectomy) and the tissue is immediately examined for cancer (frozen section examination).
- The prostate is fully exposed and then the urethra is cut between the tip of the prostate (apex) and the pelvic floor.
- The two vas deferens are severed and the seminal vesicles are separated from their bed.
- The last connection above the prostate at the neck of the bladder is cut.
- The prostate, urethra, seminal vesicles and vas deferens are removed as a single block.
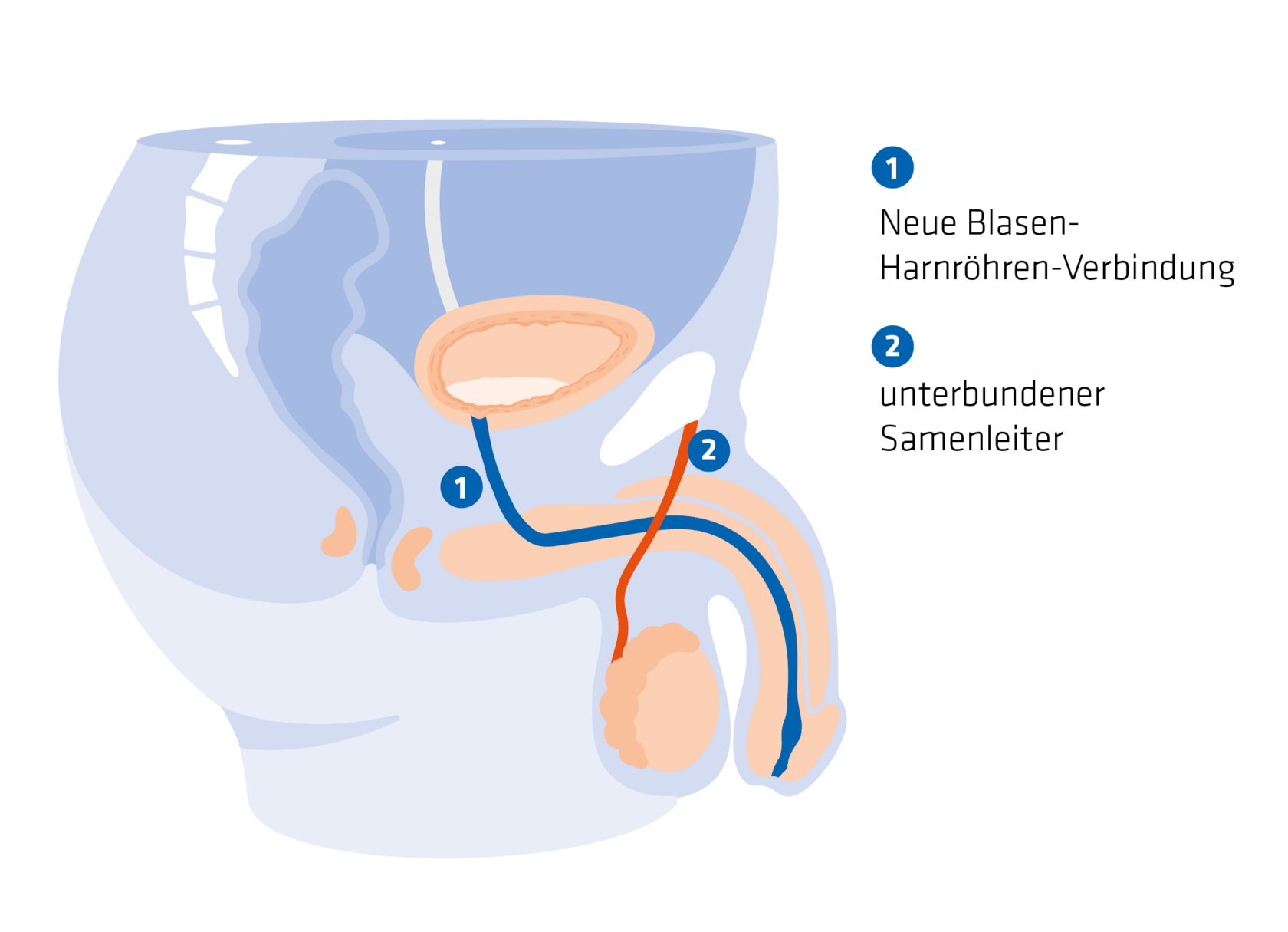
- The urethra is then sutured to the bladder neck using an in-situ catheter (anastomosis).
- If necessary, some more lymph nodes are removed and wound drains are inserted.
- The wound is closed.
The procedural details for other techniques is different. If possible, the doctors operate without damaging the nerves in order to retain the nerves and blood vessels on both sides of the prostate.
Alternatives to surgery:
It is not always necessary to treat prostate cancer immediately with surgery. Depending on the individual situation and the progression of the disease, other treatment options such as active monitoring or radiotherapy may also be considered.
Other Prostate surgeries: What are TURP and TUIP?
Good to know: There are 2 other types of prostate surgery that are not used for prostate cancer, but may be considered for benign prostate enlargement:
- Transurethral resection of the prostate (TURP): This procedure is intended for treating benign prostatic hyperplasia (BPH). A surgical instrument is inserted through the urethra to remove parts of the prostate tissue, leaving the prostate capsule intact.
- Transurethral incision of the prostate (TUIP): Also intended for treating benign prostate enlargement, tissue is cut at the bladder neck and the prostate without removing prostate tissue to make more space for the urethra.
Risks
What are the possible consequences of a prostatectomy?
As with any surgical procedure, there are potential short-term and long-term consequences of prostate surgery that need to be considered.
The success of the treatment and the risk of side effects depend on several factors:
- Age and comorbidities: Younger and healthier patients generally have a better chance of recovery.
- Surgery performed after initial diagnosis or relapse of disease (recurrence): The chances of success tend to be higher if prostate surgery is performed after initial diagnosis.
- Experience of the operating doctors: Treatment by experienced surgeons in specialised clinics can reduce the risk of complications.
- Stage and aggressiveness of the tumour: The stage at which the tumour is detected and its aggressiveness play a decisive role in the oncological success of the surgery. Tumours that are detected early and are less aggressive can generally be treated more successfully, while advanced and aggressive tumours require more complex therapy and can increase the risk of relapse.
Short-term and long-term side effects of surgery
Various side effects can occur immediately after prostate surgery:
- Pain: Post-operative pain is common and can usually be treated well with painkillers.
- Slight bleeding: Slight bleeding may occur after prostate removal.
- Infections: The surgical wound or the bladder may become infected.
- Urinary incontinence: Almost every patient experiences involuntary urine discharge after prostate surgery.
The long-term side effects of a prostatectomy depend on how extensive the surgery was and which procedure was used.
Urinary incontinence and urinary dysfunction
A common long-term side effect is urinary incontinence that causes uncontrolled urination. It affects on the average:1
- 3 months after the surgery: 50 per cent of patients
- 18 months after the surgery: 4 to 21 per cent of patients
- Long-term urinary incontinence: 10 to 15 per cent of patients
More about Urinary incontinence
Erection problems (erectile dysfunction)
Erection problems are another potential side effect of prostate removal. Most patients experience them for a short time after the surgery - but the function often recovers to the level before the surgery if the surgeon has been careful with the nerves. In around 19 to 40 per cent of patients, erectile dysfunction persists for a long time.1
The sensation of touching the skin (for example on the penis) and the libido remain unaffected by prostate surgery . However, ejaculation is no longer possible as all the necessary organs are removed. However, men still retainthe ability to orgasm - this is referred to as a "dry ejaculation", in which sperm is no longer released.
Loss of fertility
Due to the removal of the prostate, seminal vesicles and vas deferens, ejaculation is no longer possible and those affected can no longer conceive naturally. Men who wish to have children should therefore find out about the possibility of freezing sperm (cryopreservation) before the surgery.
Post-surgical care
What happens after prostate surgery?
After the prostatectomy, the patient initially remains in the recovery room or intensive care unit for a few hours for monitoring before being transferred to the normal ward. Drinking is usually permitted on the day of the surgery; food intake is started gradually once the bowel starts working again. The day after the surgery, the patient can usually get up with the help of the nursing staff.
Hospitalisation
The bladder catheter remains in the urethra for a few days until the sutures at the anastomosis (connection between the urethra and bladder) heal and the swelling in the area of the urethra subsides. The wound drains are usually removed after about 3 days. Hospitalisation lasts from a few days to 2 weeks, depending on the procedure.
Between the 3rd and 10th day after the surgery, the condition of the anastomosis is checked by X-ray examination after injecting a contrast medium into the bladder (cystography). If it is not leaking, the in situ catheter can be removed .
Rehabilitation and post-surgical care
Rehabilitation and post-surgical care programmes begin a few weeks after the surgery. These are designed to support recovery and alleviate potential long-term side effects.
Ideally, rehabilitation begins immediately after you are discharged from hospital. It can take place on an inpatient or outpatient basis and include the following services:
- Continence training
- Sport and exercise therapy
- Counselling and treatment for erectile dysfunction
- Psycho-oncological care
- Legal advice on rights to get support in everyday life and at work
- Disease-specific counselling by a urologist
the PSA (prostate-specific antigen) value is checked 4 to 6 weeks after the prostate surgery. It should then be in the "undetectable range" (below 0.2 ng/ml). The value is checked again within 6 to 12 weeks. An increase in the PSA value may indicate remaining tumour or metastases, which then necessitates further treatment.
Regular check-ups are recommended in order to identify any potential relapse of the disease at an early stage - especially in the first 5 years after the surgery.
Digital support
In addition to conventional rehabilitation measures, there are now digital support options, such as the prostate app Uroletics, which was developed by urologists at Munich University Hospital together with physiotherapists.
FAQ
Frequently asked questions and answers about prostatectomy
Prostatectomy is a surgery to remove the prostate. The technical term for the complete removal of prostate, including the seminal vesicles and vas deferens, is radical prostatectomy (RPE).
The prostate is completely removed if prostate cancer is diagnosed and the cancer is still confined to the prostate. Removal of the prostate can also be considered for locally advanced prostate cancer.
There are different types of prostate removal: open (retropubic by making an incision in the lower abdomen or perineal by making an incision in the perineum) and minimally invasive (laparoscopic with a keyhole surgery) methods.
The aim of radical prostatectomy is to treat prostate cancer. The chances of recovery are good if the surgeon manages to remove all the tumour tissue.
During a radical prostatectomy, the entire prostate, the seminal vesicles, the vas deferens, part of the urethra and the internal sphincter muscle are removed. If necessary, the nearby lymph nodes are also removed.
Possible side effects and long-term consequences of prostate removal are urinary incontinence and erectile dysfunction. Incontinence can be improved by exercising the pelvic floor muscles. Erection problems can vary depending on the type of surgery.
After radical prostatectomy, ejaculation is no longer possible as the vas deferens and seminal vesicles are removed. However, the ability to orgasm remains unaffected. Those who have undergone the surgery have a dry discharge where sperm is not released.
Healing after prostate surgery varies. It usually takes several weeks to months for the patient to fully recover. Pelvic floor muscle exercises and rehabilitation programmes can help the healing process.
Hospitalisation after a prostate surgery usually lasts a few days to a maximum of 2 weeks, depending on the surgical procedure and the healing process.
After prostate surgery, regular check-ups are necessary to ensure that all cancer cells have been removed and there is no relapse. The PSA value is checked regularly. Rehabilitation measures such as continence training, exercise therapy and psycho-oncological care help in recovery and to minimise long-term side effects.
Sources
- 1 “Therapy for prostate cancer: Radical prostatectomy". Cancer Information Service, German Cancer Research Centre, https://www.krebsinformationsdienst.de/prostatakrebs/operation. Accessed on 05 July 2024.

![[Translate to English:] Mann blickt zufrieden in die Kamera: Die Prostatektomie ist eine Therapieoption für seinen Prostatakrebs.](/fileadmin/_processed_/f/3/csm_AdobeStock_211651043_7fa0d3db67.jpg)