Symptoms
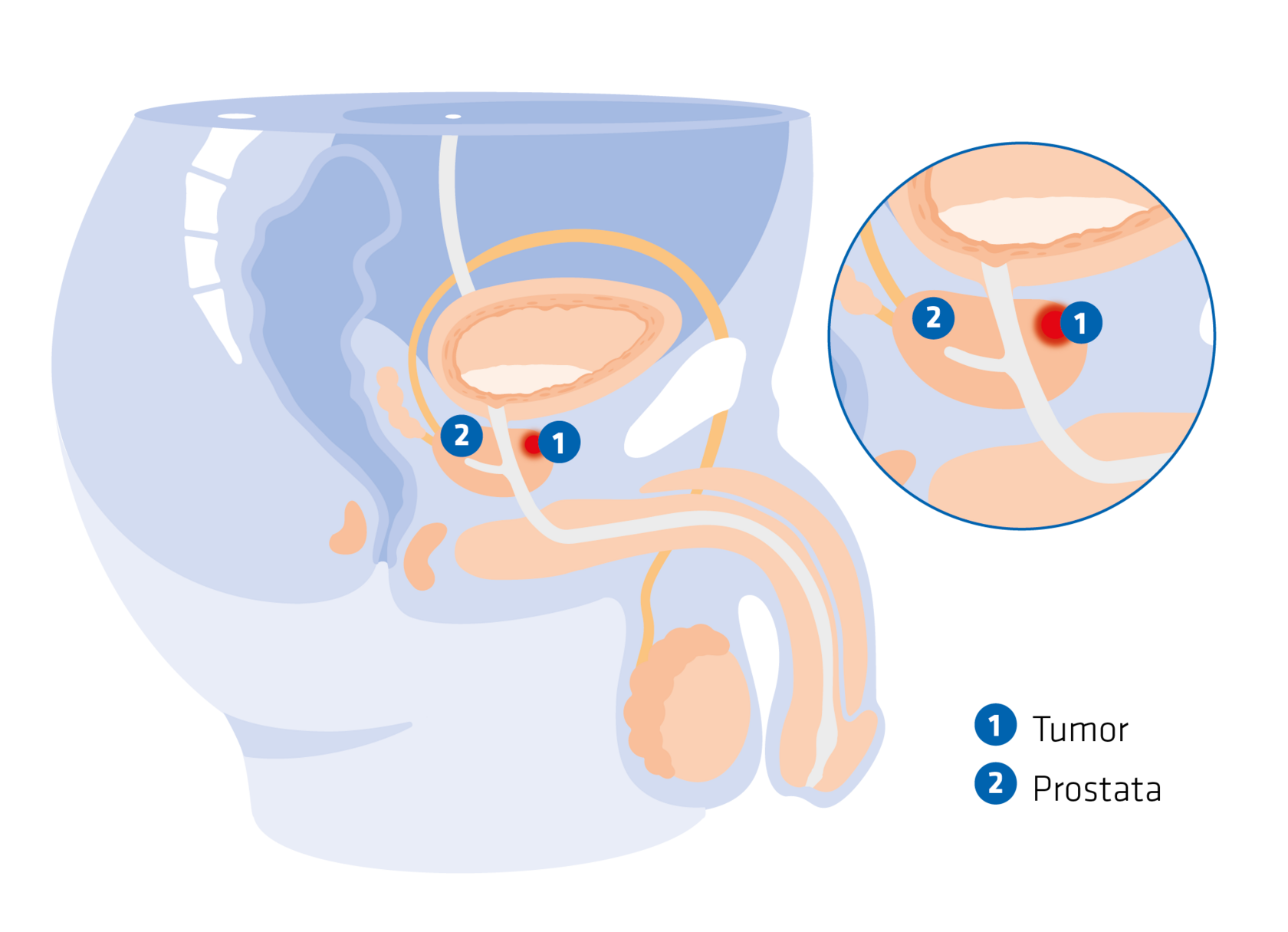
Symptoms and progression of prostate cancer
In the early stages of the disease, symptoms are rarely noticeable. Prostate cancer often develops in the outer (peripheral) regions of the prostate and only constricts the urethra when the cancer is already very large or has spread. In case of prostate cancer, the following symptoms can indicate an advanced stage:
- Weak urine stream
- Urinary stuttering
- Dribbling after urination
- Frequent urination
Other symptoms such as rheumatic pains and reduced performance as well as blood in the urine or semen can also occur.
Sciatica and bone pain can be caused by secondary tumours (metastases). Acute impotence may also indicate the presence of prostate carcinoma.
Good to know: prostate carcinoma (prostate cancer) is not the same as benign prostatic hyperplasia (abbreviated as: BPH). BPH is benign prostate enlargement. It is a normal physiological process in men, as the prostate grows steadily from the age of 40. The abbreviation BPS is also used in addition to BPH. The term benignprostate syndrome refers to the symptoms associated with benign prostate enlargement.
How frequently does prostate cancer occur?
In 2020, around 65,820 new cases of prostate carcinoma were diagnosed in Germany. Men rarely have prostate cancer before the age of 50. For example, a 35-year-old man has a less than 0.1 percent chance of being diagnosed with prostate carcinoma in the next years, while a 75-year-old man has a 6.7 percent chance over the same period.1
Trigger
Causes and risk factors of prostate cancer
The causes of prostate cancer are still unclear. The risk factors are:
- Age
- Family predisposition
- Hormone status
- Unhealthy lifestyle (smoking, alcohol, nutrition)
It is not yet known whether obesity can also increase the risk of prostate carcinoma. However, there is evidence that a lack of physical activity can increase the basic risk of cancer.
Diagnosis
How prostate cancer is diagnosed
The earlier prostate carcinoma is diagnosed, the better are the chances of treatment and even recovery. The following tests can be carried out to diagnose prostate cancer:
- Digital Rectal Exam (DRE): the urologist feels the prostate by putting his finger through the rectum and can feel benign enlargements, suspicious lumps and hardenings.
- Transrectal Ultrasound (TRUS): images of the organs of the pelvis (prostate, seminal vesicles, urethra) are created using ultrasound so that the doctor can see the size, shape and structure of the prostate as well as any abnormalities.
- Determination of the PSA value: PSA stands for prostate-specific antigen. This protein is produced by the prostate cells. A value between 0 and 4 nanograms per millilitre (ng/ml) is considered normal. An increase in this value (> 4 ng/ml) may indicate prostate carcinoma. If the value exceeds 10 ng/ml, doctors suspect the presence of prostate carcinoma.
To confirm a diagnosis of prostate cancer, a biopsy is carried out on an outpatient basis in a clinic or in a specialist urological practice. To do so, the doctor removes the prostate tissue either through the rectum (transrectally) or through the perineum (perineally) using a hollow needle. The tissue is removed under local anaesthesia. The microscopic examination of the tissue samples taken reveals within a few days whether prostate carcinoma is present and how the tumour can be classified. The classification is important because the treatment is based on it.
According to current guidelines, a multiparametric MRI (mpMRI) should be performed before a biopsy or after a biopsy if the diagnosis is not clear. In this new imaging procedure, a combined image of various tissue properties is created using a contrast agent, leading to a more precise diagnosis.
Classification of prostate carcinoma
As part of the diagnosis, prostate cancer is classified according to the so-called TNM system.
The following three criteria are decisive for this:
Primary tumour (T) T0: not detectable T1-T4: increasing size and penetration depth of the primary tumour | Lymph node involvement near the tumour (N) N0: no lymph node involvement N1-N3: increasing lymph node involvement | Distant metastasis (M) M0: no distant metastases M1: distant metastases detected |
Treatment
The treatment of prostate cancer is always carried out on a case-by-case basis
The treatment recommended by the doctor after the diagnosis of prostate cancer depends on the results of the biopsy (tissue removal) and the spread of the tumour (size, location, lymph node involvement, metastasis) and must be adapted to the patient's personal situation (age, physical condition, personal wishes). The main options for the treatment of prostate cancer are:
![[Translate to English:] Arzt diagnostiziert bei einem Patienten ein Prostatakarzinom und berät ihn zur Behandlung.](/fileadmin/_processed_/c/3/csm_AdobeStock_593478476_e99eb0cb2f.jpeg)
- Active surveillance: If the cancer is not in a very advanced stage yet and is growing slowly, treatment may be delayed for the sake of quality of life under strict monitoring. In such cases, doctors only start treatment when certain values (e.g., the PSA value) indicate that the prostate cancer is progressing, or when the patient requests it.
- Watchful waiting: if doctors are of the opinion that the prostate cancer will not cause any problems during the patient's lifetime, the tumour can be monitored over the long term and palliative treatment (aimed at alleviating the symptoms) can be started if necessary. This is an option, for example, if an affected man is already very old and/or has other concomitant diseases.
- Surgery (radical prostatectomy): when tumours are limited to the prostate, radical prostatectomy, abbreviated as RPE, is the method of choice for permanent cure. The entire prostate, including the tumour, is removed together with the spermatic ducts and the seminal vesicle. The chances of recovery are very high: studies show that 7 out of 10 men are cured after a radical prostatectomy.2 However, the risk of recurrence increases if the cancer is already so advanced that complete surgical removal of the tumour is no longer possible.
- Radiotherapy: as an alternative to surgery, prostate carcinoma can also be treated with radiotherapy. The radiation of the prostate can be done either from the outside through the skin or from the inside, by doctors placing small radioactive metal needles in the prostate.
- Anti-hormonal therapy (hormone therapy): Hormone therapy is suitable for men whose prostate cancer is no longer localised to the prostate but has already metastasised, i.e., spread to the lymph nodes or organs that are farther away. Since, in many patients, prostate cancer grows under the influence of the male sex hormone testosterone, hormone therapy aims to remove this hormone from the body or to block its effect on the cells. This treatment method can also be an option if, for some reason, surgery or radiotherapy is not possible.
- Chemotherapy (cell-killing drugs): chemotherapy is only used in the late stages of prostate cancer, when the tumour starts growing independently of hormones (castration-resistant prostate cancer). Chemotherapeutics are cytostatic drugs that inhibit the growth of cancer cells and destroy them. Chemotherapy is only of limited use for prostate cancer because prostate cancer cells grow slowly.
Targeted therapies: in combination with other therapies, targeted therapies (such as PARP inhibitors) can also be used for prostate cancer. Unlike chemotherapy, these drugs act more specifically on the cancer cells (targeted) and therefore have fewer side effects. Whether and which treatment is appropriate depends on the tumour, the patient's general condition and previous treatments.
It is also possible to combine certain therapies. For example, if the cancer has already spread from the prostate to other organs at the time of diagnosis, surgery or radiotherapy alone is not enough. Additional treatments, such as hormone therapy, are then usually used.
How can you be a part of the healing process?
Many people who are diagnosed with cancer find it a drastic and "life-changing" experience. Seek psychosocial counselling or make use of psycho-oncology services if you are experiencing extreme emotional distress. This can help you cope with the emotional and social challenges that cancer brings.
All therapies more or less affect your sexual interest and potency. This can lead to misunderstandings with partners. Talking openly with your partner is the only way to manage your illness successfully and perhaps open new ways of achieving a fulfilling relationship.
An intact immune system is also important. So, make sure you eat a balanced, healthy diet. Exercising in fresh air can also have a positive effect on your general well-being. Light and regular endurance sports are ideal for this.
Make appointments for check-ups so that any progression of the tumour can be detected and treated quickly.
Prevention
Prevention of prostate cancer: early detection is important!
Preventive check-ups help in the earliest possible detection of existing illnesses. Half of all cancers could be prevented or diagnosed at an early stage and thus permanently cured if those affected avoided risk factors (such as smoking, alcohol or poor diet) and attended early detection screenings regularly. Prostate cancer is also easier to cure when detected early.
![[Translate to English:] Mann hat sich über Vorsorge zu Prostatakrebs informiert und steht zufrieden in der Küche.](/fileadmin/_processed_/f/3/csm_PCa_Website-01-Diagnostik_e82b98c79d.jpeg)
All legally insured men aged 45 and above are entitled to a free preventive urological check-up every year. It includes one consultation with the doctor, where the doctor asks about any complaints. A urologist also examines the reproductive organs and the lymph nodes in the groin and feels the prostate through the rectum (Digital Rectal Exam). However, because tumours that are either unfavourably located or still very small are likely to go undetected, it is better to do a PSA test as well. The level of the protein that is only produced in the prostate (prostate-specific antigen) can also indicate a possible prostate carcinoma at a very early stage.
Important: increased PSA concentration in the blood can also be seen in men, who have benign prostate enlargement or an infection of the prostate. Multiple PSA values should therefore be taken over a period of time.
Specialist groups
Prostate cancer: information for specialist medical groups
To access detailed product information on the treatment of advanced hormone-dependent prostate carcinoma after using the specialist group login, click here:
Downloads
Free service material on prostate cancer
Download free service material on the subject of prostate cancer here:
FAQ
Answers to frequently asked questions about prostate cancer
In case of advanced prostate carcinoma, the symptoms can include weak urine stream, urinary stuttering, dribbling after urination or frequent urination. Symptoms such as rheumatic pain, reduced performance, blood in the urine or semen, sciatica, bone pain and acute impotence can also occur.
No. Prostate carcinoma (prostate cancer) is a malignant tumour in the prostate. BPH (benign prostatic hyperplasia) is a benign prostate enlargement. Doctors use the term BPS (benign prostate syndrome) when talking about the symptoms of benign prostate enlargement.
In Germany, around 65,820 men were diagnosed with prostate carcinoma in 2020.1 Men are rarely affected by this cancer up to the age of 50.1 Thereafter, the probability of developing prostate cancer increases with age.1
The causes of prostate carcinoma are still unclear. However, there are some factors that probably contribute to the development of the disease: age, family predisposition, hormone status and an unhealthy lifestyle (smoking, alcohol, nutrition).
There are several tests that doctors can use to diagnose prostate carcinoma: Digital Rectal Exam (DRU), Transrectal Ultrasound (TRUS), determination of the PSA value or biopsy (removal of prostate tissue).
Prostate-specific antigen (PSA) is a protein produced by the prostate cells. Increased levels of PSA in the blood can indicate the presence of prostate carcinoma.
If palpation (Digital Rectal Exam (DRE)) and/or Transrectal Ultrasound (TRUS) are abnormaland/or an increased PSA level is detected, a biopsy (removal of a tissue sample) is recommended to provide clarity.
The treatment of prostate carcinoma depends on various aspects, such as whether the tumour has already affected other organs in addition to the prostate. Common treatment options include active monitoring, watchful waiting, surgery, radiotherapy, anti-hormonal therapy, chemotherapy and targeted therapies.
If the prostate cancer has progressed and formed metastases (secondary tumours), localised treatment is no longer enough. Systemic (affecting the whole body) hormone therapy is then recommended. It prevents the prostate carcinoma from increasing in size and spreading.
Support your immune system with a balanced and healthy diet and regular sporting activities. Take your appointments for check-ups seriously. Talk openly to your partners and seek professional help if you are experiencing severe emotional stress.
In order to detect prostate cancer at an early stage, when it is still easily curable, men over the age of 45 should regularly undergo the preventive annual urological check-up, which is offered free of charge by statutory health insurance companies. This usually includes one consultation with a doctor, a Digital Rectal Exam (DRE) and a PSA test.
Sources
- 1 Cancer in Germany 2019/2020. 14th edition. Robert Koch Institute (ed.) and the German Cancer Registries - GNCR (formerly known as Association of Population-based Cancer Registries in Germany) (ed.). Berlin, 2023.
- 2 “Treatment in early stages". Krebsgesellschaft.de, https://www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/krebsarten/prostatakrebs/therapie/behandlung-im-fruehstadium.html. Accessed on 8 July 2024.
- 3 “Prostatakrebs (Prostatakarzinom)” (Prostate cancer (prostate carcinoma)). German Centre for Cancer Registry Data (ZfKD) at the Robert Koch Institute, https://www.krebsdaten.de/Krebs/DE/Content/Krebsarten/Prostatakrebs/prostatakrebs_node.html. Accessed on 19 June 2024.

![[Translate to English:] Mann mit Prostatakrebs schaut dank seiner Behandlung optimistisch in die Kamera.](/fileadmin/_processed_/a/2/csm_PCa_Website-Titelbild_v2_1def994b31.png)
![[Translate to English:] Ärztin im Gespräch mit einem Patienten über Prostatakrebs.](/fileadmin/_processed_/e/e/csm_PCa_Website-04-Vorsorge_d5472d37b8.jpeg)